This site is intended for Healthcare Professionals only. if you are a member of the general public, click here
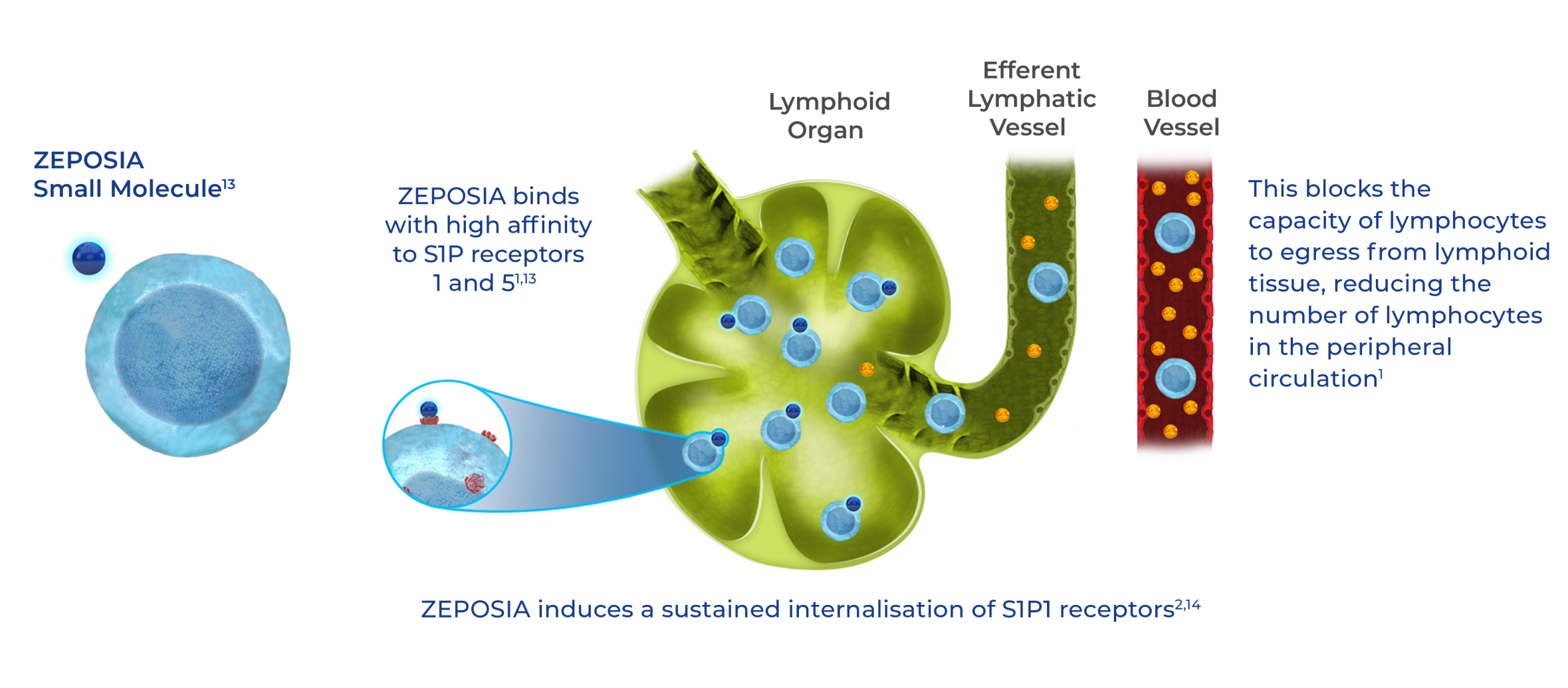
How does ZEPOSIA work?
 Pinch & zoom to explore
Pinch & zoom to explore
- ZEPOSIA targets S1P receptors 1 and 5 to help reduce gut inflammation1-3
- The mechanism by which ZEPOSIA exerts therapeutic effects in UC is unknown but may involve the reduction of lymphocyte migration into the intestine1
- ZEPOSIA has minimal or no activity on S1P2, S1P3, and S1P4 receptors1
- ZEPOSIA has minimal impact on monocytes, natural killer and natural killer T cells, which are all involved in innate immune response – a key component of immunosurveillance against infection and tumours1,15
S1P, sphingosine-1-phosphate; UC, ulcerative colitis.
References
- Zeposia (ozanimod) Summary of Product Characteristics, 2022.
- Scott FL et al. Br J Pharmacol 2016; 173:1778–1792.
- Sandborn WJ et al. NEJM 2021; 385(14):1280–1291
- Peyrin-Biroulet L et al. Autoimmune Rev. 2017;16:495–503.
- Schwab SR, Cyster JG. Nat Immunol. 2007;8:1295-1301.
- Jaigirdar SA et al. Front Immunol. 2017;8:1627.
- Karuppuchamy T et al. Mucosal Immunol. 2017;10:162–171.
- Schwab SR et al. Science 2005;309:1735–1739.
- Roviezzo F et al. J Pharmacol Exp Ther. 2011;337:830–837.
- Danese S et al. J Crohns Colitis 2018;12(suppl 2);S678–S686.
- Suh JH et al. Transl Cancer Res. 2015;4(5):469–483.
- Proia RL, Hla T. J Clin Invest. 2015;125:1379–1387.
- Lucaciu LA et al. Eur J Gastroenterology & Hepatology 2020:32;669-677.
- Lamb YN. Drugs 2020;8:841–848.
- Harris S et al. Neurol Neuroimmunol Neuroinflamm 2020; 7:e839.



